Content Warning: I’m going to share some moments from our time in the NICU. It may be difficult for some people to read. Proceed with caution.
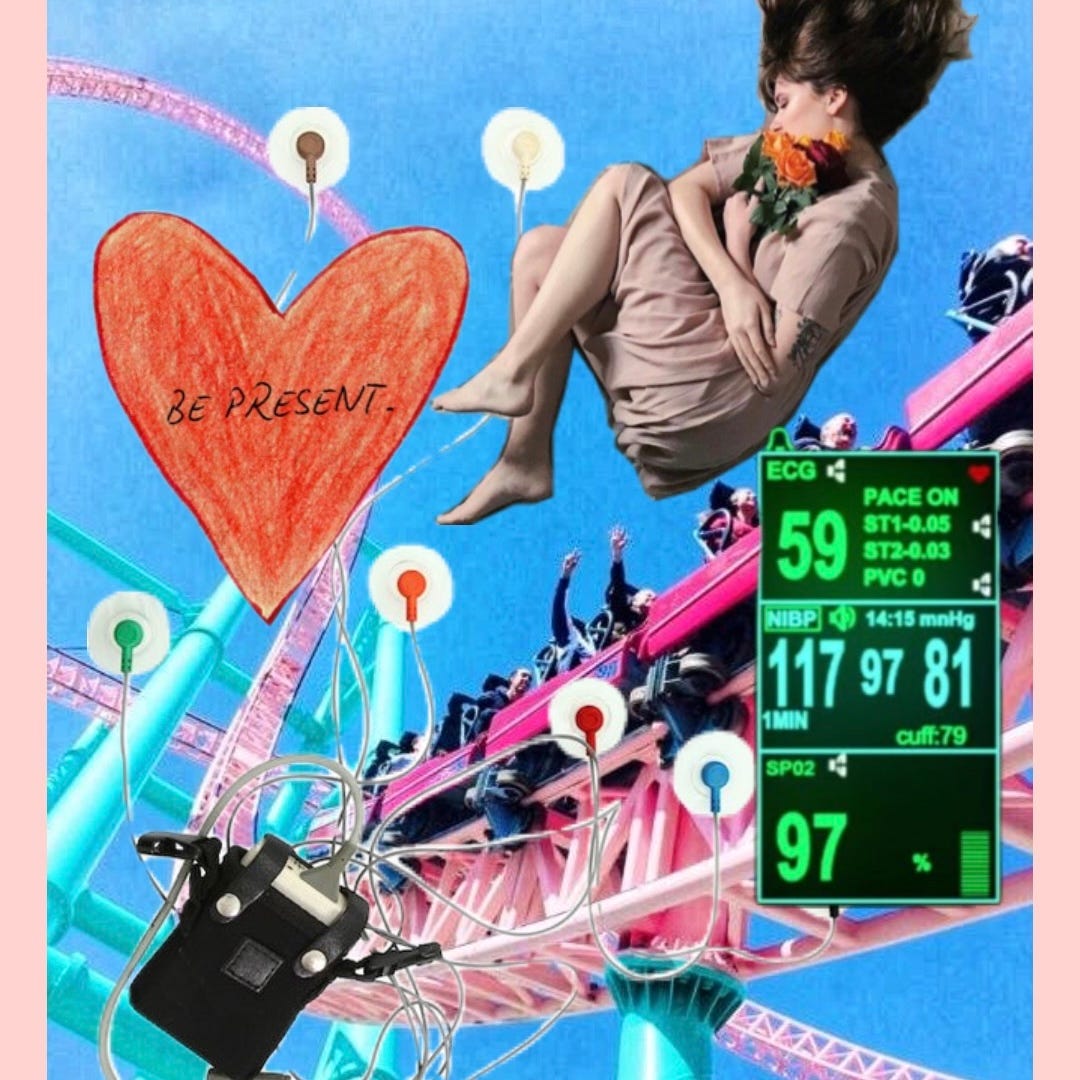
A roller coaster. A spaghetti noodle. Whiplash. All things I’ve heard have been described as being a parent in the Newborn Intensive Care Unit (NICU). We experienced the NICU for 104 consecutive days. We never were able to take our baby home. Her bassinet is left assembled in our bedroom, undressed. Each time we returned home at night during those 104 days, we saw the baby items scattered around our apartment, wishing one day we were going to be the lucky parents to take our NICU baby home.
According to the CDC, as of 2025, about 10% of infants are admitted to the NICU. This number increased by 13% in the past ten years. The highest birth rate is among mothers who are either below age 20 or above age 40. Upon reflection, I would say this is very true. A lot of the other parents I saw seemed to be older or younger than my husband and I, who are in our early thirties. It’s a weird thing to relate to when you see other parents because you know their babies are sick too. When we were there, we couldn’t help but wonder why other babies were in the NICU and if it was like our situation. Some babies, we learned, needed a new heart, or were born premature with lung disease. Some were born needing intense surgeries to be done days after they were born. Several twins were born with one requiring more support than the other. I would envy the families where their baby had something fixable. Even needing a new heart meant their baby could be saved. My baby couldn’t be saved. Even if she recovered, she would struggle with the rest of her life.
The first few NICU days are the most raw. The day after I gave birth and we came home, seeing her bassinet staged and ready for a baby, I broke down. I was in pain and devastated. My baby was taken from me, and she was sick. We had no idea what was wrong with her. I kept telling myself, “She’s in the safest place she could be.” But each time we had to say goodbye at the end of the day, I would cry beside her bed. I didn’t want to leave her. That’s how the first couple of weeks went. We would wake up as early as possible, drive an hour to the hospital, and spend all day with her. For the first week, my husband would push me through the halls in a wheelchair as I couldn’t walk comfortably following the birth.
The nurses are amazing. It’s simply an understatement. I hear this every time I read about someone talking about the NICU, but it’s true. When I was holding my daughter in her final moments, her nurse was crying with us, and I told her we loved her. She had nursed our daughter a few times prior in the months us being there. We knew her well, and she was such an attentive and kind nurse. I’m so grateful that she was there with us for those last moments. I felt safe with her there. I wish I could give her the world. She made the worst day of my life bearable. And that sentiment reflects over so many of the other nurses there. So many of them made us feel welcomed and supported. I have a stack of thank you cards next to my keyboard, and I wish I could write a thank you note for all the nurses we had.*
You expect when you have a baby, to be able to freely hold them, feed them, and change their diaper. In the NICU, you need to ask permission to do any of that. A lot of the time, the baby is on a schedule. For our daughter, she ate and was changed every three hours. She had heart, lung, and oxygen monitors attached to her, as well as various IVs throughout the time. My brother-in-law compared the diaper change my husband was doing to “diffusing a bomb.” Taking care that none of the cords were to land in the poop. I was fortunate enough to be able to breastfeed my baby. Not many babies in the NICU eat enterally. Many are given feeds through a nasogastric tube that is taped to their cheek. Our daughter had an NG tube because a lot of the time she wouldn’t finish her required amount of feed, but she loved eating. She would eat from bottles very well. It was some of our favorite moments with her. When I breastfed, there was a little more production. Because she had to take a certain volume, we had to weigh her before and after she ate, holding her cords in the air and then, when she ate, maneuvering them so nothing was pulling so she could breastfeed comfortably. Honestly, the experience deterred me from wanting to breastfeed. It would stress both of us out more than not. The scale would only read if she were staying still. If she’s a hungry baby, she’s squirming and crying, even when I put blankets on the scale to make it softer. Eventually, we would have skin-to-skin moments after she was bottle-fed instead. Still to this day, I can feel the weight of her lying on my chest and her soft hair brushing along my lips as I’d lean down to press a kiss to her head.
Even though we lost our daughter, I am grateful for all that we were able to do with her while she was in the NICU. Since we were there for so long, I saw the state of other babies. So many were hooked up to life support in the form of breathing tubes and incubators. For the most part, my husband and I could come in, and if she was lying there, we were comfortable enough to pick her up and hold her. We became very familiar with maneuvering the IV and monitor lines without any issues. The nurses knew us well and knew we were independent parents. Such a funny thing to say about being a parent. That we didn’t need help to care for our baby.

A roller coaster is the best way I could describe being in the NICU because the visceral reaction you have while riding a coaster is mirrored as a parent in the NICU. There were days it felt so normal. She wouldn’t need any interventions and was pretty stable. We would feed her, change her, and cuddle. We’d be able to go home and feel relaxed knowing she was fine. They had baby cameras that we could watch while at home to see her either sleeping or looking directly into the camera. And on other days, we’d arrive to find out she'd taken a turn for the worse, or a lab result would come back abnormal, or something that meant she needed extra help. A lot of NICU babies develop Necrotizing Enterocolitis (NEC) because it affects preterm or low birth weight babies. Our daughter developed this two weeks into being in the NICU, and after this point, she needed further intensive care from then on. It was such that for her to go home, she would have to survive without interventions.
At one point, we didn’t go home. There were a few times we would request a sleep room and stay the night. I’ll start by saying that I’m very grateful that our hospital has sleep rooms available to families. Not all hospitals have them. However, the accommodations were lackluster. I’d compare them to maybe a 2-star motel—gross showers with pink discoloration on the floor, beds resembling cardboard with one thin blanket atop. You had to be out of the room by 8 am. But it was something that allowed us to be close to her when we were nervous about her stability. The longest we stayed at the hospital was for about 10 days straight after her labs came back, saying her liver was in failure. We were told she only had days to live. She ended up living another 6 weeks. She was a fighter, up until the end.
When a baby in the NICU has an event, their monitor starts blinking red or blue and makes an intense, repetitive beeping sound that alerts every monitor in the area. If the nurse assigned to the baby needs help, they hit the code button. An announcement is made over the hall with the location of the room. Every nurse stops what they are doing and runs to the room to help. Nearly every staff member and doctor stops what they are doing and goes to the room with the chest compression machine and anything to help the baby. We witnessed several babies around us in code blue events. It’s a highly stressful moment. Sometimes the baby recovers on their own without any help, but others need intense aid to revive them. Our daughter did not have a code event. In the final days of her life, it was clear her body was shutting down. If she were to be revived, it wouldn’t be a bridge. So as we saw her numbers decrease on the screen, the intense beeping accelerated, drowning out the sound of my sobs, the nurses came in and turned off the monitors and beeping. We didn’t have anyone rush in; we were with her in her last days, the three of us holding on to one another, peacefully being in our final moment as a family of three.
Leaving her room, we were in for the last time, was the strangest feeling. We had been in that particular room for about two months. The hospital we were in had three wings of level four NICU, which is the highest level of care for infants and newborns. If your baby is very sick, you go to this hospital. It’s one of the best in the country. We were lucky enough to live within driving distance, but the hospital felt like our home, too. We would put her footprints up on display like art pieces and stack books along the wall. I’d have clean outfits in a drawer ready for her to be dressed each night after her bath. It was our home. Before that, we were in ‘pods’. Larger rooms with four to five babies in the room. There were times I think they did things for us because they didn’t think our daughter was going to survive. So they would make us as comfortable as possible. They’d get us two comfy chairs for our room, even though the rule was only one chair per bedside. They moved us to this private room within a day of it being requested, even though we later learned there is a waitlist for the private NICU rooms. I have to think it’s because we were there every day. We saw some parents there; some came every day, but usually only for a couple of hours. Some we only saw once a week or once a month. We were fortunate enough not to be working and able to be there for her nearly every waking moment.
We were highly involved in every round with the doctors. I would recite her entire medical history to every new rotating attending physician. We would correct them if we heard anything, and we’d mention any change in her health. We were locked in. There are a handful of doctors in the NICU whom we loved working with. Some cared so much for us and wanted the best for our daughter. Alternatively, we were met with doctors who were not as hopeful, and we felt we had to fight for her care. I leapt out of my comfort zone, contacting external doctors, directors, and medical professionals to get her medicines and care. I raised my voice at doctors, challenging them that they are supposed to provide the best care, and I had yet to see it from them. We went against some doctors' suggestions and, in doing so, gained more time with our daughter.
The NICU is a surreal experience. Now, three weeks later, I cannot believe I went through all of that. It felt like a living nightmare. I never want to relive that, and I am thoroughly concerned about every parent who will continue to go through the NICU. I yearn to help. I yearn to be the support for those parents who need it. Because, especially in those early days, I needed that support.
If you are reading this and your child is in the NICU, here are some of my top tips to help make things a little easier:
Ask for your social worker assigned to your child; they should get you parking passes, meal vouchers, and information on grants that can help cover rent and other bills.
Ask if your hospital has sleep rooms/nearby lodging/laundry services. If you are staying the night, it’s nice to be able to get your clothes cleaned.
Ask if there are other parent areas in the hospital. Sometimes, the NICU will have lounge areas, but some hospitals have family centers that can be another area to take a break from the bedside without going too far.
Ask if your NICU has a psychologist to talk to if you are really struggling. We wish we had gotten a hold of our psychologist sooner because in the event of extreme distress, we felt like we were alone.
There are other departments like Speech Therapy (to help with eating), Physical Therapy (who can get your child toys), and Child Life Specialists (who can make footprint crafts) that help enhance the experience with your child.
If your child is in the NICU and you need someone to talk to, I’m here for you. You can leave a comment or message me, and I will be that person you need who relates to you—a person who understands this unique experience firsthand. I can only hope your child has a better outcome than mine.
I felt compelled to write about my NICU experience because before then, it felt foreign. No one knows what it’s like until you are living in it. I still only scratched the surface of what we went through. Some day, I know I will share it all. I will share every moment, every raw emotion. Every email and conversation. I will share it for the world to read because our story, even though it was tragic, is one to know. If anything, to inspire others never to stop advocating for the ones you love.
xoxo Anjelica
*Our hospital, where we were, offers a Daisy Award. You can nominate a nurse who helped you. In our time, I nominated two nurses. The nurse we had on our second and third day in the NICU, who made the experience feel less scary, and our last nurse, who was there with us through the end. She helped pack our room and walked us to our car. I wish I could see her again, hug her, and thank her.